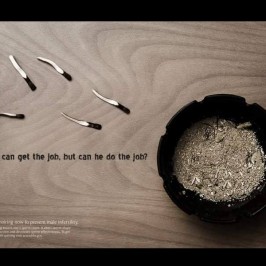
Are there options for preserving fertility in men who have been newly diagnosed with cancer?
Yes! Sperm can be collected and frozen for later use before cancer treatment is started. This way, you may be able to have children after your treatment. This process is called
cryopreservation or freezing. The kind of cancer you have and the treatments you will receive can determine what your options are.
What is involved in sperm collection?
For many men, collecting sperm to freeze is a simple, noninvasive procedure. You will be shown to a private room, asked to masturbate to orgasm, and collect your semen in a special container.
A usual semen sample will contain around 5-20 million sperm per milliliter and is able to be divided into several vials for storage. Often, since sperm production is affected by many factors, you may be asked to collect more than one sample. This helps to improve your chances of being able to have a child later.
What if I can’t give a sample?
Some men are unwilling or unable to collect a sample through masturbation. For these men, a special condom may be used to collect semen during intercourse.
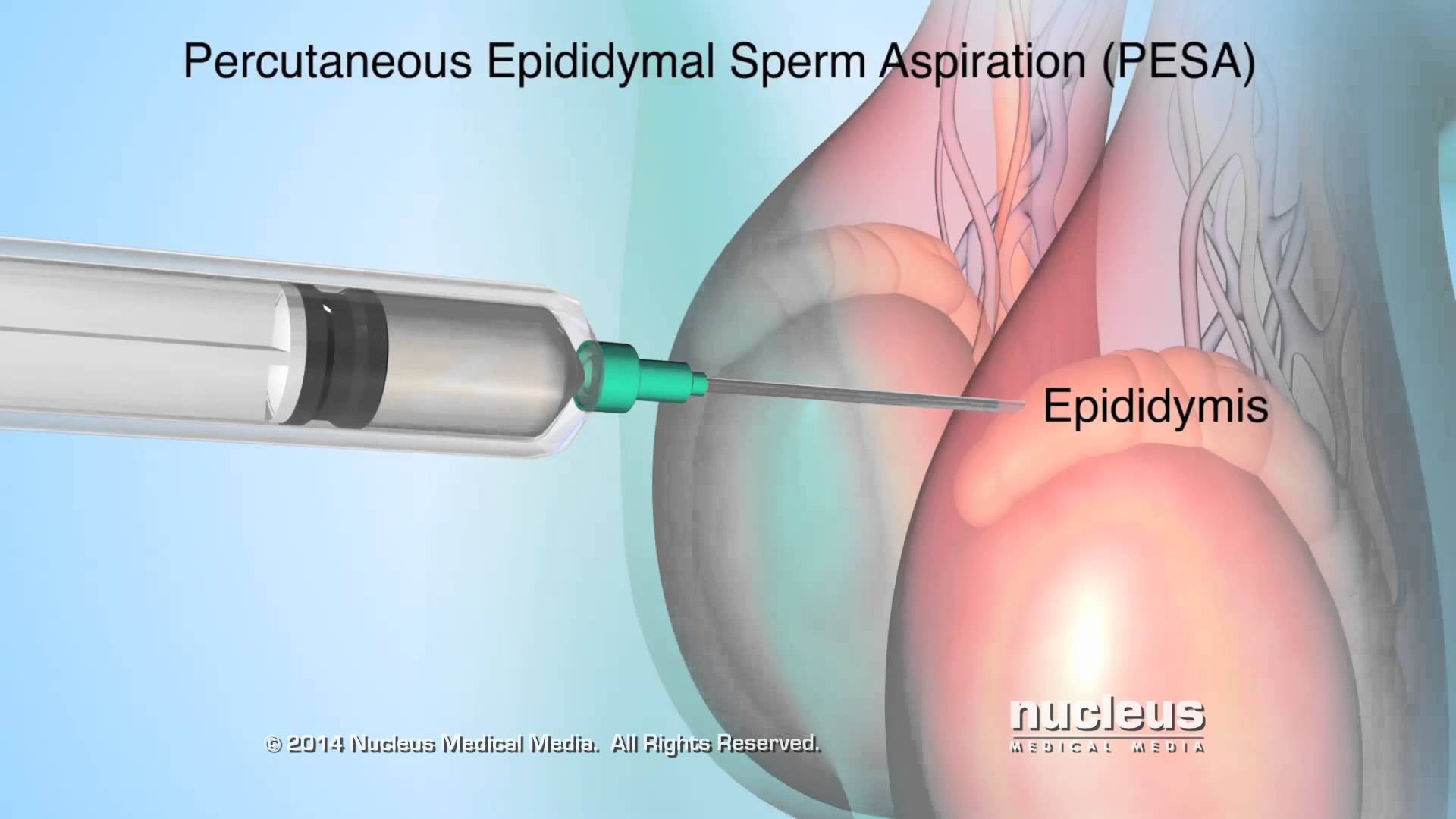
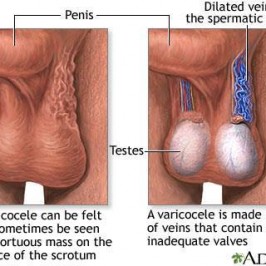
Other men have a blockage in their reproductive tract; as a result, no sperm are found in their semen. Sperm can be obtained through various procedures that remove them
directly from the testicle or reproductive tubes located beside the testicles.
Some men may have a condition that causes sperm and some or all of the semen to collect in the bladder instead of being released through the tip of the penis. For those men,
sperm can often be collected from the urine after intercourse.
If a man is unable to ejaculate (release semen durin orgasm), there are options. Sperm can be surgically removed from the testicles and injected directly into an egg in a process called intracytoplasmic sperm injection (ICSI).
If a man is not able to ejaculate due to spinal cord injury, vibratory stimulation or electroejaculation can be used.